Heel Pain? Here’s How Physiotherapy Can Help You Walk Pain-Free
Discover the common causes of heel pain, effective treatment options, and how physiotherapy can support your recovery.
Struggling with heel pain that won’t go away? Whether it’s a sharp pain in the morning, discomfort when walking, or aching heels after exercise, heel pain can disrupt your daily life and training routine. The good news is that physiotherapy can help—and the sooner you address the issue, the better.
At Movement Laboratory, we specialise in treating heel pain, foot injuries, and lower limb conditions with evidence-based physiotherapy, strength training, and movement rehabilitation. Let’s explore the common causes of heel pain, symptoms to watch out for, and how to fix it for good.
What Causes Heel Pain?
Heel pain is not just a foot problem—it’s often linked to movement patterns, muscle imbalances, and lifestyle factors. Some of the most common causes include:
Plantar Fasciopathy (Plantar Fasciitis)
This is one of the most common causes of heel pain, affecting runners, athletes, and people who spend long hours on their feet. The plantar fascia, a thick band of tissue along the bottom of your foot, can become inflamed from overuse, improper footwear, or tight calf muscles. The result? Sharp, stabbing pain under the heel, especially in the morning.
Fat Pad Syndrome
Your heel has a natural fat pad that cushions impact when walking or running. Over time, excessive strain—such as standing for long periods or repetitive high-impact activities—can cause the fat pad to wear down, leading to dull, aching pain in the heel.
Achilles Tendinopathy
The Achilles tendon, which connects your calf muscles to the heel bone, plays a key role in walking and running. Overuse, poor foot mechanics, or tight calves can lead to Achilles tendinopathy, causing pain and stiffness at the back of the heel.
Calcaneal Stress Fracture
A stress fracture of the heel bone (calcaneus) is a common overuse injury in runners, dancers, and high-impact athletes. Unlike acute fractures, stress fractures develop gradually due to repetitive loading, often causing worsening pain with activity and relief with rest.
Retrocalcaneal Bursitis
This condition occurs when the bursa (a fluid-filled sac behind the Achilles tendon) becomes inflamed due to repetitive friction or pressure. It leads to swelling, redness, and tenderness at the back of the heel, often aggravated by shoes with a rigid heel counter.
Experiencing heel pain? Get a professional assessment with our team at Movement Laboratory. Book an appointment today!
Recognising the Symptoms of Heel Pain
Heel pain can present in different ways depending on the cause. Some common symptoms include:
- Sharp, stabbing pain in the bottom of the heel (classic sign of plantar fasciopathy).
- Aching or bruised sensation in the centre of the heel (common with fat pad syndrome).
- Tenderness and stiffness at the back of the heel, especially in the morning (a sign of Achilles tendinopathy).
- Pain that worsens with running, jumping, or standing too long.
- A feeling of pressure or heaviness in the heel, particularly after exercise.
If your heel pain is persistent, getting worse, or affecting your daily routine, it’s time to seek expert treatment before it leads to long-term problems.
How Physiotherapy Can Help Heal Heel Pain
The key to treating heel pain isn’t just resting and hoping it goes away—you need a structured plan to address the root cause and prevent future issues.
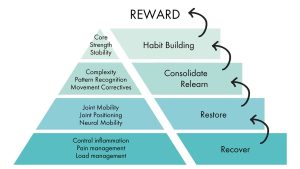
At Movement Laboratory, we follow a structured recovery framework designed to reduce pain, restore function, and build long-term resilience
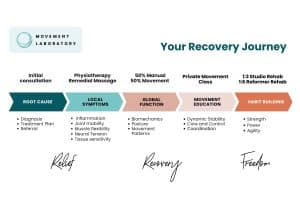 Step 1: Recover – Reduce Pain and Inflammation
Step 1: Recover – Reduce Pain and Inflammation
In the early stages, our focus is on controlling inflammation, pain relief, and managing load to allow the heel to settle. This may involve:
- Manual therapy (joint mobilisation, soft tissue release, dry needling) to relieve tension.
- Taping or bracing to offload pressure from the heel.
- Load management strategies to modify training or daily activities.
Step 2: Restore – Improve Mobility and Biomechanics
Once pain is under control, the next step is restoring joint and tissue function. This involves:
- Improving foot and ankle mobility through joint mobilisations and stretching.
- Correcting gait mechanics to distribute pressure evenly.
- Strengthening the calves, plantar fascia, and intrinsic foot muscles to improve resilience.
Step 3: Relearn – Address Movement Patterns and Stability
Many heel pain conditions stem from poor biomechanics or muscle imbalances. We work on:
- Postural adjustments to optimise weight distribution.
- Foot, hip, and core strengthening to support alignment and prevent compensations.
- Movement education to ensure proper technique in daily activities and exercise.
Step 4: Habit Building – Strength and Long-Term Prevention
The final phase is building strength, endurance, and long-term habits to prevent recurrence. This includes:
- Progressive strength training for the lower limbs.
- Sport-specific or activity-specific conditioning for athletes.
- Ongoing monitoring and follow-ups to ensure lasting results.
We don’t just treat symptoms—we guide you through a comprehensive rehabilitation processto get you back to pain-free movement. Learn more about physiotherapy at Movement Laboratory.
Preventing Heel Pain: What You Can Do
The best way to stop heel pain from returning is to build strength, improve mobility, and manage your activity levels. Key prevention tips include:
- Wear proper footwear with arch and heel support.
- Strengthen your calves, feet, and lower limbs regularly.
- Avoid sudden increases in running or high-impact activities.
- Incorporate stretching and mobility exercises into your routine.
- Address foot or muscle imbalances early before they become chronic issues.
Ready to Fix Your Heel Pain?
Heel pain can be frustrating and limiting, but you don’t have to put up with it. Whether you’re dealing with plantar fasciopathy, Achilles tendinopathy, or another foot-related condition, our expert physiotherapists at Movement Laboratory can help.
- Book an appointment now and start your recovery journey today.
- Learn more about physiotherapy and how we treat lower limb conditions.
- Join our movement classes to build strength, flexibility, and resilience.
Don’t wait until your heel pain gets worse—take action today and get back to pain-free movement!